Being your own advocate is so important, but it does come with a learning curve. In this post, I describe my not-so-great second Remicade infusion experience so you don’t have to learn the hard way to be your own best advocate.
Keep reading so you can avoid the experience I had and go into your infusions as a confident, strong, and knowledgeable self-advocate.
My Nurse’s Behavior Made Me Nervous
My second infusion was in March 2015, two weeks after my first loading dose. (Patients typically receive infusions every eight weeks, but when first starting out, you have to introduce it to the body slowly which is usually done at weekss two, six, and then every eight weeks.)
So for this second introductory infusion, I strode confidently into the hospital. My first one went extremely well and I was feeling AMAZING from the Remicade.
After the usual weigh-in, the technician escorted me back to the patient lounge. I was hoping I’d get the same lovely nurse as the time before, but I was paired with a different nurse today.
As she was prepping me for pre-meds, I was slightly taken aback. She seemed scatterbrained and chatty to the point where she kept interrupting herself. Her hands flew across the table, dropping items and plastic wrappings everywhere.

My confidence level dropped a little because she had to ask other nurses questions about my pre-meds and the equipment needed. But I ignored the onset of nerves and waited as she gathered all the materials and answers she needed.
Pre-Meds: When Things Started to Go Wrong
I swallowed the Tylenol pills with ease and was ready to insta-sleep from the syringe-given Benadryl. But instead of giving me the Benadryl from the hand-held syringe, like at my first infusion, the nurse poked me several times and then hooked me up to the IV machine.
I’d eventually have to get set up with it anyways for the Remicade—this was just an alternate way of getting the Benadryl into my bloodstream.
Once I was finally attached to the IV, she linked it with the Benadryl. And here’s the thing: When you’re hooked to the IV on the machine, there’s a dial where you can choose the rate at which the medications are pumped into your veins.
With my little experience and knowledge, I had no idea what was about to happen when she nonchalantly turned the dial up all the way.
Passing Out from the Benadryl
Very quickly, everything started turning bright. It began with fuzzy light dots overcoming my peripherals and making their way toward the center of my vision.
I felt like my head was filled with nothing but air, and it seemed to detach from my body and float away.
My fingers, hands, arms, legs become heavy, burdened by the weight of themselves.
As I started to lose consciousness, I remember becoming extremely nauseous as my head nodded to the side, unable to stay upright.
The nurse came running over in a panic turning off the dial and asking if I was okay. I don’t think I answered. She then grabbed equipment to check my vitals, which of course, resulted in her reading my extremely low blood pressure.

“You’re hypoglycemic!” the nurse exclaimed. “We can’t give you the Remicade today, you need to go to the ER!”
WHAT!? This news helped me slowly wake up—still nauseous and lightheaded—and thoughts clouded my mind. No, I need Remicade to keep me on track…I think I might throw up…Why did she turn the dial up so high?
Still in a frenzy, the nurse hurdled over to her supervisor to ask her what to do. She suggested she call my gastroenterologist to ask for her direction. Another nurse brought me juice and I waited in that chair for what felt like forever as they tried to get a hold of my doctor.
Once they finally got her on the line, she told the nurse exactly what I was hoping she would: to let me rest until my vitals return to normal, give me the Remicade (because I really needed to get it in my system!), and take me to the ER afterward to check on the possible hypoglycemia (low blood sugar).
The Remicade Infusion Itself
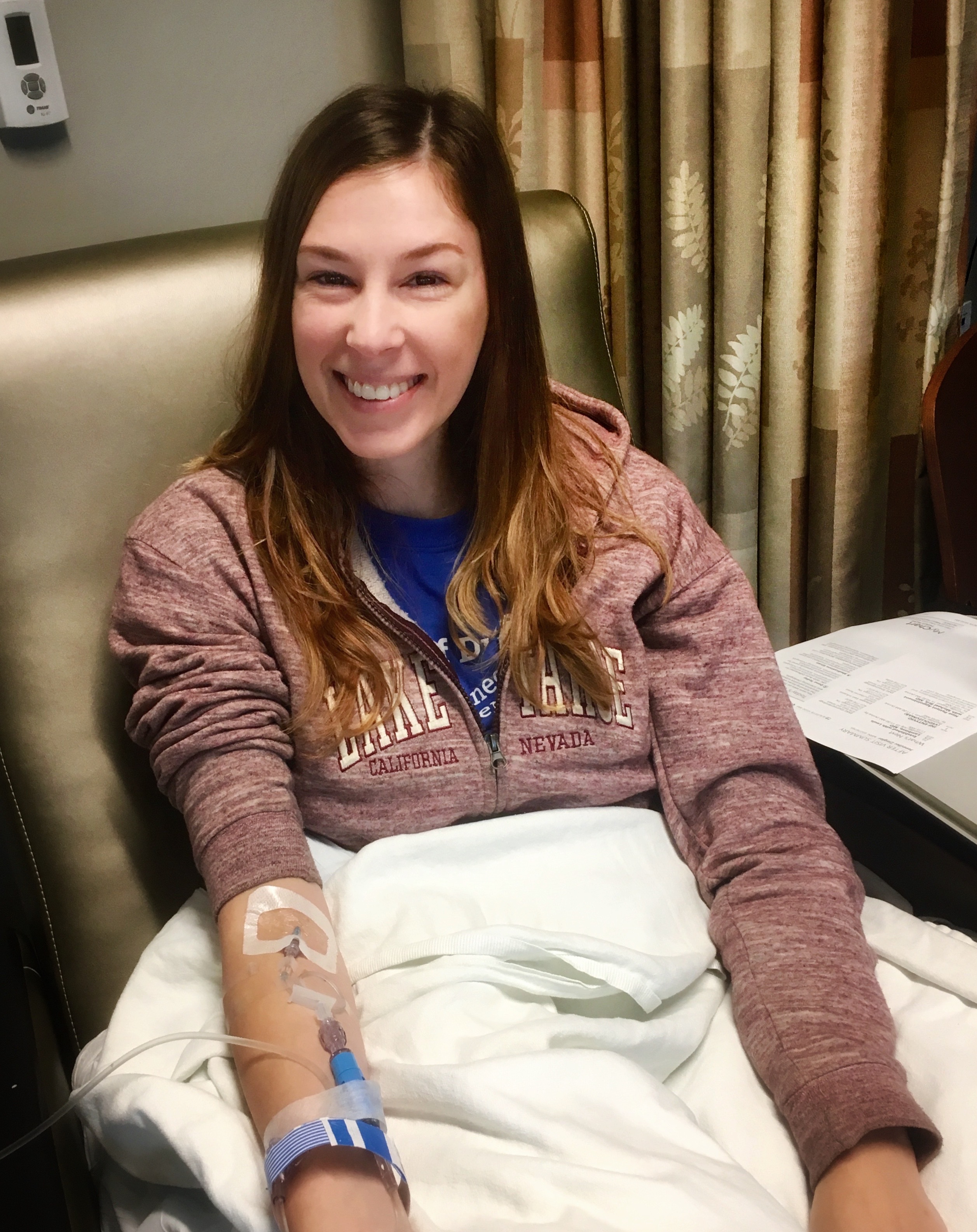
Phew. Sigh of relief. I was getting my Remicade today. After sitting a while under the blankets letting everything return to normal, they took some blood samples for testing and cleared me for the Remicade.
The infusion itself went well, but I was on edge every time the machine would beep, alerting the nurse to increase the rate for my Remicade. I knew I shouldn’t be nervous about that part—it wasn’t the Benadryl, after all. Yet, I watched with wary eyes, analyzing the nurse’s every move, unable to fully relax because I felt like I had to keep track of every button she pressed.
This infusion wasn’t nearly as peaceful as the last one.
Thankfully, the process was completed without any other hiccupsres. But now I couldn’t leave to go back to my apartment on campus; I had to go to the ER to get my blood sugar checked out.
They escorted me in a wheelchair downstairs (at least the ER was in the same building as the infusion center!), dropped me off, wished me luck, and left me all on my own.

At the Emergency Room for Possible Hypoglycemia
Uhhh. What am I supposed I do? I’m in this busy room filled with white coats flurrying by, clipboards clacking, and beeping monitors echoing throughout the space. Lost. Out of place.
I explained my situation to the man at the window, and he had a technician lead me back to a hospital bed. I changed into a gown and a doctor strapped buttons and monitors throughout my body: chest, ribs, back, fingers. I can’t remember everything he did, but the process took a while as he ran the tests.
After the testing was done, I was released from the hospital bed, but I wasn’t allowed to leave until they got the results.
This was the part that took forever; I was there for the rest of the day. Bored out of my mind. Frustrated I was here in the first place for something I’m fairly certain was NOT hypoglycemia and NOT my fault. Worried about the financial cost this trip would incur.
Hey, at least they had free sandwiches…
The Test Results
Finally, at the end of the day, the energy in the room started to die down. There were fewer patients and doctors now, and I was starting to think they had forgotten about me.
After a bit more (frustrated) waiting, they finally located me and gave me the results.
“You’re not hypoglycemic,” the doctor explained. “But you experienced a hypoglycemic episode, likely caused by too much Benadryl too fast.” So it was drug-induced low blood sugar.
Remind me to ask for a different nurse if I’m paired with her next time, I thought to myself. He also suggested to eat protein with breakfast and not just carbs to help avoid future situations like this.
They released me from the ER and I drove back to campus annoyed, let down, and exhausted. It was a long day, but at the end of it, at least I had Remicade in my system.
5 Tips to Be Your Own Advocate on Remicade
That was a long day. I learned a lot though, including some ways for me to stand up for myself for future infusions. Here are some of the lessons I learned that you can implement to help ensure you have a positive infusion experience.
1. Go Easy on the Benadryl
You can ask the nurse to dose you the pre-meds slowly. Every single infusion after my second one, I told the nurse to please give me the Benadryl at an extremely slow pace. I shared this experience with them each time, and they always understood.
Some hospitals may give the Benadryl orally, so this may not be as much of an issue. But if you get it intravenously, ask them to go slow, and you can also request that they give it to you via syringe instead of the automatic IV machine.
2. Raise Any Benadryl Concerns to Your GI Doctor
If you feel that the dosage of Benadryl is too high, bring it up with your gastroenterologist.
My second infusion was my only experience passing out from the Benadryl, but in future infusions, I’d still become lightheaded and very nauseous.
Once I told my doctor about this, she cut the dosage in half, which made a world of difference in future visits.
3. Weigh Yourself at Home the Morning of Your Infusion
By doing this, you know how much you weigh that day and you can calculate how much Remicade you should be getting at that particular infusion. (Remicade is dosed based on your weight).
Remember, the formula is: Remicade Dosage = [Your prescribed Remicade dose in milligrams] x [Your body weight in kilograms]
At this time, I weighed 125 pounds (57kg) and was receiving 5 mg of Remicade per kg. So, 57 kg x 5 mg/kg = 285mg of Remicade per infusion.
If your scale only gives pounds, take your weight in pounds and divide by 2.2. This is your weight in kg.

4. Confirm Your Details on the Medication Bag
Before they start infusing the Remicade, ask the nurse to show you the med package. Ensure that it says:
- Your name,
- The correct drug name, and
- The correct dosage that you calculated above
5. Communicate With Your Medical Team
Being your own advocate is all about open communication with your nurses and your doctor. If you have any concerns, questions, don’t hesitate to bring them up to your team. Communication is key, so don’t be shy when it comes to your health!
Remember, Patients Have Power
These are some ideas about how to be a confident self-advocate.
I’m not saying that nurses or doctors are incompetent.
What I am saying is you can help ensure you receive the best treatment possible when you are equipped with knowledge so you can communicate your concerns and desires.
This second infusion was not a fun experience for me, but it was a great learning experience that taught me lessons that I carry with me to this day.
Don’t hesitate to stand up for yourself, especially when it comes to your health, safety, and quality of life.
You are empowered!
Related Posts
My nurses seemed incompetent at my first infusion yesterday. They didn’t weigh me at all. They were all learning a new computer system and most of them had no idea what they were doing.
Oh no! I’m so sorry to hear that! I’ve heard that happens sometimes — when I was on Remicade, I would always weigh myself right before I left for the appointment and calculate the amount of Remicade I should be getting based on my weight. I’m glad the monitored your blood pressure though. Good for you for asking them to recheck 🙂 Don’t be afraid to ask them to give you the pre-meds. Or, it might be better to inform your GI they didn’t give them to you, and your GI can call them and tell them to give them to you for all future infusions. One thing IBD and Remicade, in particular, taught me is to be my own advocate. Don’t feel bad telling them what you need.