In December 2023, my world tipped upside down.
I was just coming out of a six-month ulcerative colitis flare. One day, it felt like a literal bowling ball had lodged itself in my upper abdomen.
It hurt to move.
It hurt to eat.
It hurt to breathe.
The only thing that gave me some relief was laying in bed on my left side.
After a few days of the pain refusing to subside, I went to the hospital and was admitted for three days. Little did I know, I would be hospitalized twice more that month and would receive a new diagnosis of autoimmune pancreatitis.
In this 6-part blog post series, I share my autoimmune pancreatitis diagnosis story, an overview of my three hospital stays, how I’m managing the disease now, the thing that most likely triggered this immune reaction, and how this diagnosis has impacted my ulcerative colitis treatment management plan.
So get comfy, grab a snack and a yummy beverage, and let’s dive in.
First of All, What is Pancreatitis?

Pancreatitis is inflammation of the pancreas. The pancreas is an organ located behind the stomach, nestled in-between the spleen, gallbladder, liver, bile ducts, and the top of the small intestine.
The pancreas produces hormones (like insulin) to help control your blood sugar levels; it also produces digestive enzymes (like lipase and amylase) and sends them into the small intestine to break down food.
When your pancreas is inflamed, these functions become impaired. In fact, what often happens is the enzymes spill out into the bloodstream and actually start digesting the pancreas itself, causing pain, nausea, and other difficult symptoms.
My Pancreatitis Symptoms
Symptom 1: Three Types of Stomach Pain
The first and most significant symptom I noticed was the pain. What’s strange is I experienced three very different types of abdominal pain, each at various locations and different severities. Here are the three types I experienced, ordered from most to least severe.
Stomach Pain #1: The Bowling Ball
This pain was by far the most intense. The best way I can describe the pain is that my stomach just felt heavy—like a bowling ball was trapped inside. My belly felt heavy and crampy, like a brick was sitting atop my organs. I remember standing in my kitchen, stomach relaxed and unflexed, feeling like a bowling ball was stuck inside me. It was a horrible feeling—knowing that my stomach was empty of food, and yet, something dark and heavy lurked inside.
Stomach Pain #2: The Pinching Pain
This pain was in my upper, center abdomen (above the bowling ball) just below my breastbone. Randomly throughout the day, I’d get these “pinching pains” where it felt like tiny little pincers were pinching me. Sometimes, when the pains were more intense, it felt like someone was driving a sewing needle in and out of my belly. This particular pain was a sharp, stabby pain that occurred sporadically throughout the day with no warning.
Stomach Pain #3: The Twinges
This pain occurred between the first two—somewhere between my belly button and breastbone. It felt like someone was snapping a rubber band inside my stomach, and the pain would spasm and ricochet from within. Like the pinching pain, these twinges happened randomly and without warning.

None of these pains felt anything like ulcerative colitis and I knew for a fact this was not an IBD flare.
Things that made these pains worse included eating, taking deep breaths, putting pressure on my stomach (coughing, sneezing, laying on my stomach), and moving in any way that straightened my stomach (walking, standing up straight, and lying flat on my back.)
Another thing that hurt REALLY bad was driving over bumps in the car. Even the smallest dips in the road would cause severe pain, and I had to brace my stomach to protect it whenever I saw a bump coming up in the road.
Symptom 2: Loss of Appetite and Weight Loss
Eating significantly increased the pain. Even small snacks and fibrous food caused immense heaviness, crampiness, and stabbiness, so my body went into survival mode and decreased my appetite. Unfortunately, this made me rapidly drop an unhealthy amount of weight.
Symptom 3: Nausea
Though I didn’t experience any vomiting (a common symptom for pancreatitis) I did deal with extreme nausea. I felt weak and lightheaded and fought to keep the little bit of food down.
I remember being at a bookstore with my family—a place that brings me immense joy—and I had to sit down on the carpeted floor to bend my stomach and fight the nausea. I was in so much pain, I just wanted to leave the books on the shelves, go home, and lie down.
Hospital Stay #1
December 4th – 6th, 2023
After three days of these intense pains, I finally accepted things weren’t going to get better on their own and decided to go to the ER.
They did their normal blood work routine and, when I was sitting in the triage room, they came back with the shocking lab results: my lipase was 5,279 U/L! The normal range is 13 – 75 U/L!!!
They explained that high lipase is correlated with pancreatitis.
My jaw hit the floor. And I lowkey freaked out.
Pancreatitis? I thought. Doesn’t that happen when you drink too much alcohol?
(I hardly ever drank alcohol even before this diagnosis; maybe several drinks a few times a year.) But apparently, there are a whole host of things that can cause pancreatitis beside alcohol abuse.
What Can Cause Pancreatitis?
- Abdominal injury, trauma, or surgery: I’ve never had abdominal surgery, so I knew this wasn’t the reason for my pancreatitis.
- Gallstones: These are hardened bits of bile trapped in the gallbladder or bile ducts. These are usually identified by ultrasound, MRI, or CT scan.
- High levels of fat particles (triglycerides) in the blood: This can be checked in a lipid panel, a simple blood test.
- Very high levels of calcium in the blood: You can easily check your calcium levels in a CBC blood test.
- Certain medicines: Quite a few medications have pancreatitis listed as a potential side effect. It’s best to talk with your doctor about the meds you’re on.
- Infections such as mumps, hepatitis A or B, or salmonella: There are blood and stool tests that screen for these things.
- Certain genetic defects: You can test for this in a specialized 3-gene panel blood test.
- Idiopathic: This may just be the most frustrating one. Idiopathic pancreatitis is when the pancreas becomes inflamed for an unknown reason that’s never discovered.
- Autoimmune: Labs and procedures can help diagnose this. There are two types:
- Type 1 is more common. It’s associated with elevated IgG4 and can impact other organs in addition to the pancreas, such as the liver, kidneys, and thyroid.
- Type 2 is more rare, and these patients often have normal IgG4. This type only affects the pancreas and is closely associated with IBD.
Testing at the Hospital
As I waited in triage before being officially admitted to the hospital, they did a bunch of labs and procedures in an attempt to figure out the cause of my pancreatitis.
Test #1: Blood Work
- Complete blood count (CBC) and comprehensive metabolic panel (CMP): Everything was normal, including my liver function numbers and calcium levels, which ruled out calcium-related pancreatitis.
- C-reactive protein (CRP): My CRP was high at 14.9 mg/L. (The upper limit is 8 mg/L). This was expected, as pancreatitis is inflammation of the pancreas, but it did not give us any info about what was causing the pancreatitis.
- Lipid panel: This checked for high levels of fat in my blood. Everything was normal, including triglycerides, cholesterol, HDL, and LDL. This ruled out pancreatitis caused by fat levels in the blood.
- IgG4: My level was normal. It was 15 mg/dL, and the normal range is between 2 – 96 mg/dL. This ruled out autoimmune pancreatitis type 1.
Test #2: CT Scan
They also had me do a CT scan with contrast. Shockingly, my results said, “The pancreas is unremarkable.”
So, the CT scan showed no signs of pancreatic abnormality or inflammation. This confused me and the hospital team, given my insane pain levels and ridiculously high lipase.
Test #3: Ultrasound
Shockingly, again, my results said, “No evidence of acute pancreatitis or gallstone pancreatitis.” So although it didn’t note anything wrong with my pancreas, it at least ruled out the potential gallstone trigger.
Hospital Treatment Plan
Despite these tests failing to identify the reason for my pancreatitis, I was still hospitalized due to my pain and high lipase levels. I was there for two nights and three days.
The standard approach for treating pancreatitis—especially when the cause hasn’t been identified—is a two-pronged approach: pain management and bowel rest.
They gave me Dilaudid (hydromorphone), which was truly a God-send. In fact, it was one of the first things they offered me in the triage room.
I’d told them my pain was an 8 out of 10, but, like many others living with chronic illness, we have oftentimes grown so used to pain that the pain level is actually higher than we say.
Looking back, I’d consider my pain at least a 9. Honestly, this was more painful than the worst, bloodiest, crampiest ulcerative colitis flare I’ve had.
Next, they put me on NPO—meaning I couldn’t eat or even drink water. The theory is that by stopping eating and drinking, it gives the pancreas time to rest and heal.
For the next two days, I laid in the hospital bored, worried, and thirsty. Honestly, I wasn’t too hungry because of my inflamed pancreas, but some broth would have been nice! On the third day, they slowly let me reintroduce foods, starting with clear liquids, then soft foods, then, eventually, lean meat.
It was critical that I eat only a low-fat diet for the next few weeks for my pancreas to heal.
On December 6, 2023, I was released from the hospital. My lipase was still off the charts at 1,652 U/L (remember, the normal range is between 13 – 75 U/L).
It felt strange being discharged when my lipase was still high. It still hurt to eat and I was disappointed that they hadn’t figured out what was causing my pancreatitis. However, I was happy to go home and continue recovery from the comfort of my own bed.
My At-Home Treatment Plan
They sent me home with Norco and instructed me to continue eating a low fat diet. And I mean, extremely low fat—no more than 30 grams of fat per day! That’s only 5 grams of fat per meal/snack, as I was supposed to eat six small meals a day. This is basically nothing!
Next time you look at a nutrition label, check to see the product’s fat content. Even healthier pre-packaged foods like almonds or peanut butter or popcorn or veggie chips have much more than 5 grams of fat per serving. This was a shock to me, and I had to get creative when trying to find foods I could eat.
I was also instructed to drink LOTS of water. Drinking water when recovering from pancreatitis is critical because it helps flush out the pancreas, provides it with needed fluids to recover from inflammation, reduces the stress put on the pancreas, aids in digestion, and helps absorb nutrients.
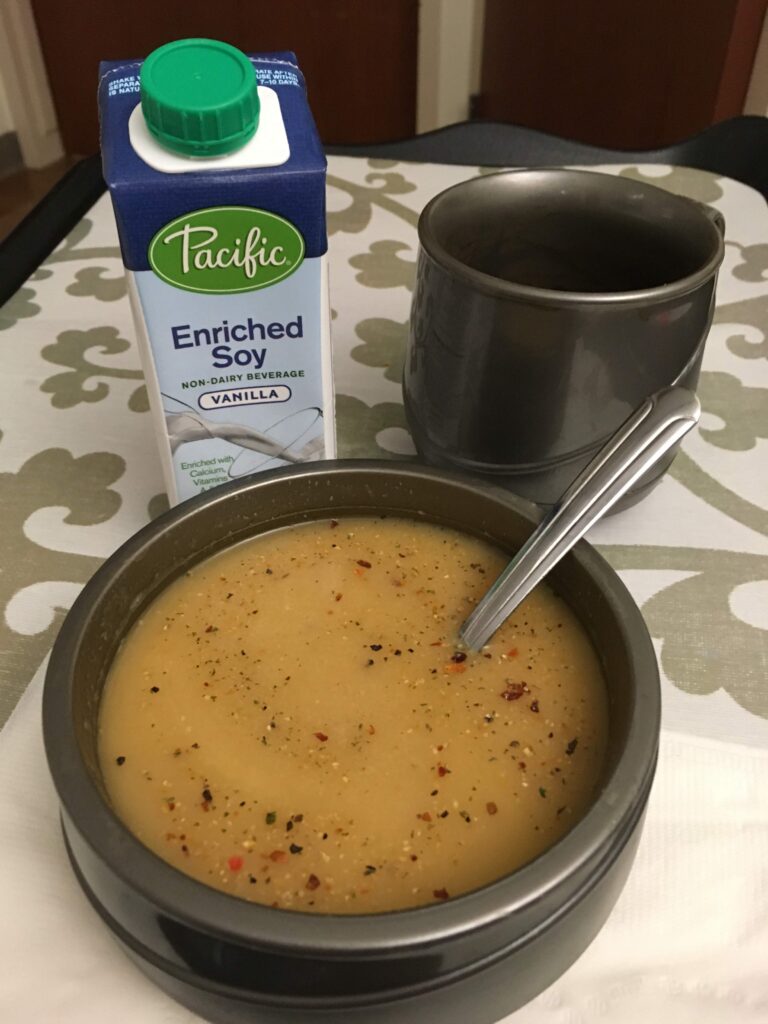
For the next nine days, I chugged water and ate low-fat foods like pretzels, crackers, broths, soups, applesauce, fruit, and Italian ice.
But instead of feeling better, I started to get worse. I knew I needed to go back to the hospital.
Read Part 2 in This Pancreatitis Series
This first hospital stay was just the beginning of this wild rollercoaster autoimmune pancreatitis journey.
Go ahead and hop over to part 2 for the next post in this 6-part series where I share about my second hospitalization, an enlightening abdominal MRI, starting digestive enzymes, and receiving an unofficial diagnosis.
Want more information on autoimmune pancreatitis, my symptoms, and this crazy diagnosis journey? I’m breaking my Instagram hiatus during this time to share lots more info about this lengthy health update. Find me on Instagram here.
Thank you for reading, and chat more soon!






Leave a Reply