Hi and welcome back to this six-part blog series about my 2023 – 2024 journey with autoimmune pancreatitis. Today is part five, but if you missed any previous posts, be sure to read them here first!
- Part 1: My first hospital stay, what causes pancreatitis, my pancreatitis symptoms and off-the-charts lipase levels, and my in-hospital treatment plan.
- Part 2: My second hospital stay, testing and procedures at the hospital, my abdominal MRI, starting a low-fat diet and digestive enzymes.
- Part 3: My Third Hospitalization, a Specialty Endoscopy, and Starting Prednisone
- Part 4: Living with Autoimmune Pancreatitis: Three Prednisone Tapers, Declining Azathioprine, and a Possible Alternative Diagnosis?
- Part 5: A Strange Doctor’s Note, Researching the Link Between Entyvio and Pancreatitis, and Stopping Entyvio
In part five, we left off this story with me deciding to stop Entyvio. This was one of the best decisions I ever made because it led to the healing of my autoimmune-related, drug-induced pancreatitis! However, it also caused my ulcerative colitis to flare even though my doctor and I had a plan in place to start Stelara.
So, I started Stelara in a horrible UC flare. But before we chat about that, I want to share why I chose to replace Entyvio with Stelara.
Considering Biologic Replacement for Entyvio
When I decided to stop Entyvio, I immediately dove into other biologic options so I could have a replacement on board.
At this time, the only other biologic I’d been on was Remicade, so that one wasn’t an option. In fact, I was leaning away from the entire anti-TNF drug class simply because they tend to have more potential liver- related side effects than other biologics. Since I already live with the rare autoimmune liver disease, primary sclerosing cholangitis (PSC), I wasn’t sure if that would be the wisest decision.
Researching the IL-23 Drug Class
I did a lot of digging into the IL-23 drug class. The full name for this is interleukin inhibitors; this drug class targets and blocks certain proteins created by the immune system that cause inflammation in IBD.
There are quite a few drugs in this category including Stelara, Skyrizi, Omvoh, and Tremfya.
Skyrizi, Omvoh, and Tremvya all target IL-23, but Stelara targets both IL-23 and IL-12. I liked this about Stelara because I found some research that blocking IL-12 could play an important role in managing AIP! So, in the off-chance that I was wrong about Entyvio causing my pancreatitis and if my pancreatitis was true autoimmune type 2 pancreatitis, I was hopeful that Stelara would help manage it.
Pro Tip: If you’re comparing different IBD medications, I recommend using the Crohn’s and Colitis Foundation’s medication guide! You can sort by drug class and learn about their mechanisms of action, safety during pregnancy, and other useful info.

I also found a few case reports about doctors prescribing Stelara off-label to manage AIP. I’d even heard anecdotal reports from patients on social media about Stelara putting their AIP in remission!
Finally, Stelara has a really great safety profile, and I felt confident that it would be a good choice for my liver.
Starting Stelara: Induction Infusion
On July 19, 2024, I had my Stelara infusion at my infusion center. With Stelara, you get one induction infusion followed by self-injections every eight weeks.
The infusion took about an hour, and I went through it with no issues. When starting a new biologic, there’s always a risk of developing side effects like dizziness, rash, shortness of breath, headaches, and other things, so the nurses checked on me regularly to ensure I was doing well. I had absolutely no issues and felt great during the whole infusion.
The day before my infusion, I chugged at least a gallon of water, so I think this helps things go smoothly! It also helped plump up my tiny veins, and the nurse was able to stick me with one poke.

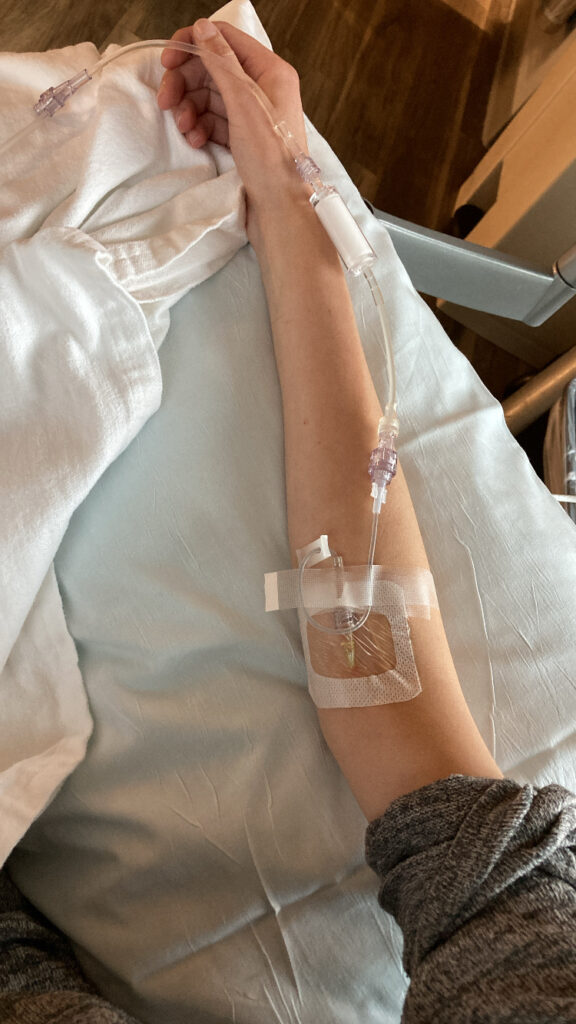

You can see in these pictures how skinny I was. I’d lost so much weight over the past months with my restrictive low-fat diet, and I was so ecstatic to start Stelara. I was hopeful it would get my ulcerative colitis into remission so I could finally get my life back.
First Stelara Injection
My first self-injection came eight weeks later. At that point, I was feeling okay. I was definitely still flaring, but I was doing better than I was at the time of my infusion. So, it was either the Stelara infusion or the prednisone (or both) that was helping.
By the time of this first injection, I had tapered back down on prednisone and was at 10 mg. This is a nice, low dose that would help tell us if Stelara works or not.
For my first injection on September 13, 2024, I had my Nurse Navigator through the Stelara With Me program come to my house to demo how to use the syringe. Even though I’m not scared of needles, I’ll admit, looking at the Stelara syringe was a bit intimidating because the needle is quite long.
I did a few practice injections with the dummy injector, and then finally did the actual injection in my stomach. It went so smoothly that I thought I must have done something wrong! It was helpful having the nurse and my husband watch and be my cheerleaders as I slowly plunged the needle into the fat of my stomach.



That day, I was a happy camper, feeling hopeful that my pancreatitis was now in the past and that I was on the road to remission with my ulcerative colitis.
Conclusion
Thanks for joining me on this wild ride as I shared my pancreatitis journey in this six-part blog post. I hope you never have to go through pancreatitis yourself—but if you do, I hope you find this information helpful.
This time during 2023 and 2024 was incredibly tough for me, filled with many canceled plans, physical pain, emotional days. Thank you to everyone who has supported me during this time. It truly means so much!






Leave a Reply